Product Description
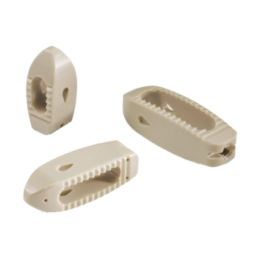
This self-distracting posterior interbody fusion device is designed to facilitate efficient, versatile and reproducible spinal fusion procedures. The name Ardis, Greek for “point of an arrow,” well suits this system whose implant has a “ double-bulleted” nose providing for an easier insertion. This multipurpose PEEK-OPTIMA* spinal device can be used in a variety of surgical approaches including TLIFs and PLIFs and is ideal for open, mini-open or MIS techniques. Ardis, which is available in a comprehensive range of sizes and has a convex shape, facilitates an individual fit to the patient. The system also features low-profile and glare-resistant instrumentation that allows for excellent visibility during any procedure, regardless of the approach. A threaded inserter with a secondary knob for an enhanced instrument/implant connection gives the surgeon more precision, control and confidence during implantation.
Features
• Conforms to varying patient anatomy:
Convex design conforms to the concave vertebral endplates to maximize endplate contact
and allow the amount of lordosis to be customized
• One of the most comprehensive size ranges in the industry:
Ensures a customized fit due to the comprehensive range of size options that
accommodate TLIF and PLIF procedures
• Self-distracting and self-retracting:
Double-bulleted design reduces insertion forces and trauma to the endplates while
simultaneously retracting nerve roots for added neural protection
*PEEK-OPTIMA® Polymer is a registered trademark of Invibio Ltd.
ZS-SA0700-04_A

Device Description
The Ardis implant is a device for interbody fusion of the anterior column of the spine. Ardis may be used to replace the disc. These cages are hollow so that bone can grow through the device, fusing the adjacent bony surfaces.
The Ardis implant is a hollow device with texture on two opposing convex sides, and is offered in various lengths, widths and heights. Zimmer Spine designed the Ardis device to be placed through a posterior or transforaminal approach and to address vertebrae in the lumbosacral region of the spine. The system contains implants of various sizes to accommodate different patient anatomy, and instruments for site preparation, trialing, insertion and extraction.
The device is crafted from (polyetheretherketone) PEEK-OPTIMA® (ASTM F2026). As PEEK-OPTIMA is radiolucent, radiographic markers are included in the distal and proximal ends of the PEEK implants. The markers consist of tantalum wires and beads (ASTM F560) that are press-fit into small holes in the implant.
The Ardis instrumentation system is comprised of instruments and perforated instrument cases that are generally comprised of aluminum, stainless steel, and/or polymeric materials.
The instrument cases may be multi-layered with various trays, holders and silicone mats to hold surgical instrumentation in place during handling and storage.
The perforated instrument cases allow sterilization of the contents to occur in a steam autoclave utilizing a sterilization cycle that has been validated by the user for the equipment and procedures employed at the user facility. Instrument cases do not provide a sterile barrier and must be used in conjunction with a sterilization wrap to maintain sterility.
Indications
The Ardis System is indicated for use with autogenous bone graft as an intervertebral body fusion device at one or two contiguous levels in the lumbosacral region (L2-S1) in the treatment of degenerative disc disease (DDD) with up to Grade 1 spondylolisthesis or retrolisthesis at the involved level(s). DDD is defined as discogenic back pain with degeneration of the disc confirmed by history and radiographic studies. Patients with previous non-fusion spinal surgery at the involved level may be treated with the device. Patients should be skeletally mature and have had six months of nonoperative treatment. The Ardis System is implanted using a posterior or transforaminal approach and is intended to be used singly or in pairs with supplemental fixation.
Contraindications
Disease conditions which have been shown to be safely and predictably managed without the use of internal fixation devices are relative contraindications to the use of these devices.
Active systemic infection or infection localized to the site of the proposed implantation are contraindications to implantation.
Severe osteoporosis is a relative contraindication because it may prevent adequate fixation of spinal anchors and thus preclude the use of this or any other posterior spinal instrumentation system.
Any entity or condition that totally precludes the possibility of fusion, i.e. cancer, kidney dialysis or osteopenia, is a relative contraindication.
Other relative contraindications include obesity, pregnancy, certain degenerative disease, and foreign body sensitivity. In addition, the patient’s occupation or activity level or mental capacity may be relative contraindications to this surgery. Specifically, some patients may, because of their occupation or lifestyle, or because of conditions such as mental illness, alcoholism or drug abuse, place undue stresses on the implant.
Known patient sensitivity to device materials (PEEK OPTIMA).
Prior fusion at the level(s) to be treated.
Any condition not described in the indications for use.
Warnings
Following are specific warnings, precautions, and adverse effects, which should be understood by the surgeon and explained to the patients. These warnings do not include all adverse effects, which can occur with surgery in general, but are important considerations particular to metallic internal fixation devices. General surgical risks should be explained to the patient prior to surgery.
1. Potential risks identified with the use of this device system, which may require additional
surgery, include:
a) Device component fracture.
b) Loss of fixation.
c) Non-union.
d) Fracture of the vertebra.
e) Neurological injury.
f) Vascular or visceral injury.
2. CORRECT SELECTION OF THE IMPLANT IS EXTREMELY IMPORTANT. The potential for satisfactory fixation is increased by the selection of the proper size, shape and design of the implant. While proper selection can help minimize risks, the size and shape of human bones present limitations on the size, shape, and strength of implants. Use of provided trials is recommended.
3. IMPLANTS CAN BREAK WHEN SUBJECTED TO THE INCREASED LOADING ASSOCIATED WITH DELAYED UNION OR NON-UNION. Internal fixation appliances are load sharing devices which are used to obtain an alignment until normal healing occurs. If healing is delayed or does not occur, the implant may eventually break due to fatigue. The degree or success of union, loads produced by weight bearing, and activity levels will, among other conditions, dictate the longevity of the implant. Notches, scratches or bending of the implant during the course of surgery may also contribute to early failure. Patients should be fully informed of the risks of implant failure.
4. PATIENT SELECTION. In selecting patients for internal fixation devices, the following factors can be of extreme importance to the eventual success of the procedure:
a) The patient’s occupation or activity. If the patient is involved in an occupation activity that includes substantial walking, running, lifting or muscle strain, the resultant forces can cause loss of disc height and/or failure of the device.
b) A condition of senility, mental illness, alcoholism, or drug abuse. These conditions, among others, may cause the patient to ignore certain necessary limitations and precautions in the use of the appliance, leading to implant
failure or other complications.
c) Certain degenerative diseases. In some cases, the progression of degenerative disease may be so advanced at the time of implantation that it may substantially decrease the expected useful life of the appliance. For such cases, orthopaedic devices can only be considered a delaying technique or temporary relief.
d) Foreign body sensitivity. Where material sensitivity is suspected, appropriate tests should be made prior to material selection or implantation.
e) Smoking. Patients who smoke have been observed to experience higher rates of pseudarthrosis following surgical procedures where bone graft is used.
5. These warnings do not include all adverse effects that can occur with surgery in general. General surgical risks should be explained to the patients prior to surgery.
6. Patients with previous spinal surgery at the level(s) to be treated may have different clinical outcomescompared to those without a previous surgery.
Precautions
1. Prior to use, the physician should be trained in the surgical procedure recommended for the use of this device.
2. The Ardis device is a single use device and should not be reused. An explanted device should never be reimplanted. Possible risks associated with re-use of single use devices include:
• Mechanical malfunction
• Transmission of infectious agents
3. The DEVICE has not been evaluated for safety and compatibility in the MR environment. The DEVICE has not been tested for heating or migration in the MR environment.
Possible Adverse Effects
Possible adverse effects associated with general surgery include complications from anesthesia, infection, hematoma and death.
Possible adverse effects associated with laparoscopic surgery include: organ or bowel injury, peritonitis, incisional herniation, damage to blood vessels, hemorrhage, injury to the nervous system and conversion to open procedures.
Possible adverse effects associated with gas insufflation include: hypercarbia, gas embolism, retention of gas in the peritoneum, omentum or viscera or lyphocele formation.
Possible adverse effects associated with spinal surgery include: dural leaks, paralysis (complete or incomplete), sensory loss, loss of bowel and/or bladder control, retrograde ejaculation, failure of the bone to incorporate and scarring of nerve roots.
Possible adverse effects associated with the Ardis device may include: fracture of another vertebra during placement, device breakage, device migration, material sensitivity or allergic reaction, spinal cord impingement, bone resorption, loss of disc height, soft tissue damage, damage to large blood vessels and pseudoarthrosis.